Scaling Telehealth to Enable Care Continuity in Pediatric Cardiology During the COVID-19 Pandemic
By Tara L. Haskell, MBA, MHSA
Heart Institute, Cincinnati Children's Hospital
By Kori Morrison
The Center for Telehealth, Cincinnati Children's Hospital
Original Publish Date: February 9, 2021
Abstract
As a response to COVID-19, telehealth was quickly spread at our pediatric tertiary academic medical center to offset the reduction of in-person visits due to social distancing regulations. Heart Institute (HI) telehealth volumes increased by 18,100% compared to pre-COVID-19 and Cincinnati Children’s (CCHMC) hospital-wide telehealth volumes increased by 4,714% compared to pre-COVID-19. Temporary policy changes for telehealth expansion issued by The Centers for Medicare & Medicaid Services (CMS), private payors, and state licensing agencies removed barriers and empowered healthcare providers to continue care safely through the pandemic. Scaling a project of this size at an expedited rate inherently came with challenges, most notably an accelerated training process for a new care model for most physicians and putting in place a telehealth infrastructure linked to Epic. Additionally, variability in private payor reimbursement guidelines and differing state licensure requirements across provider types proved to be difficult for determining which patients were suitable for a telehealth visit.
Collaboration across the institution was vital to ensure smooth execution. Leadership and staff in Patient Services, Hospital Administration, Center for Telehealth (TCT), Access Services, Payor Relations, and Medical Staff Services (MSS) worked together to fast-track necessary changes to allow wide-spread implementation of telehealth in patient homes. As a result, telehealth will continue to be an important care delivery model for CCHMC post-COVID 19.
Background on Telehealth Utilization at CCHMC
Telehealth has been evolving at Cincinnati Children’s (CCHMC) since 2000. Initially the usage was for diagnostics but grew to include over 40 specialty care clinics. Prior to COVID-19 impacting Ohio in March of 2020, CCHMC was averaging 2,000 video visits a year with 45% of those visits taking place in the patient’s home. The telehealth activity for the Heart Institute (HI) was primarily focused on provider-to-provider consultations and case conferences. There were two (2) HI physicians specializing in Heart Failure and Electrophysiology, conducting consults with patients. However, those patients were located at external partnering institutions at the time of the consult.
Implementation Process & Timeline
Hospital-wide Scaling of Telehealth
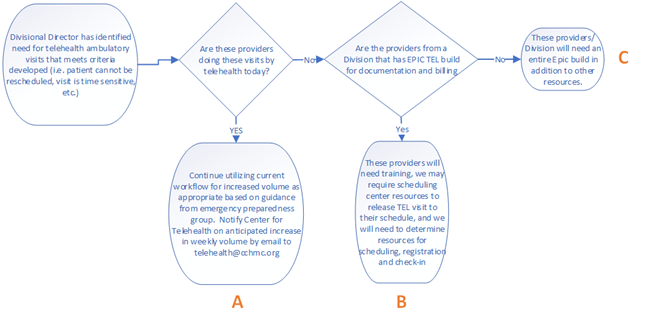
Prior to COVID-19, Centers for Medicare & Medicaid Services (CMS) defined telehealth as the utilization of technology with audio and video capabilities that are used for two-way, real-time interactive communication (Centers for Medicare & Medicaid Services, 2020). In early March 2020 a State of Emergency was declared for Ohio as a result of COVID-19 (Bischoff, 2020). Further, the definition of “telehealth” was changed by CMS and a waiver was put in place to allow for audio-only (telephone) visits to be considered telehealth (Centers for Medicare & Medicaid Services, 2020).
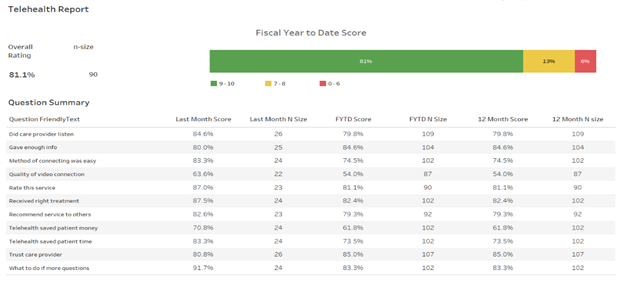
TCT worked closely with Senior Leadership to develop a scope of work focused on delivering patient care in patient homes via telehealth. Programs were categorized into groups based on their readiness to launch or scale telehealth visits quickly. Implementation readiness was driven by existence of an Epic build allowing divisions to schedule, document, and bill for telehealth visit types, as well as their level of experience utilizing telehealth [See Figure 1]. Due to provider licensure variability from state-to-state, TCT also collaborated closely with the MSS to secure temporary emergency licensure where needed.
Once program readiness was defined and technical infrastructure was expanded, an email was sent from CCHMC’s Chief of Staff to all divisions regarding the hospitals COVID-19 response and how telehealth would play a role in socially distant care continuity. The email instructed divisions to complete a request for telehealth support. Requests were reviewed, categorized based on readiness and then assigned to a member of the TCT team. A follow up document was sent to all those who requested support outlining next steps.
Cardiology Implementation [Figure 2]
During the second week in March 2020, telehealth was ramped up in the Heart Institute and across CCHMC. In total, 14 cardiology subspecialty programs launched telehealth in patient homes, including four multidisciplinary clinics: Adult Congenital Heart Disease, Cardiovascular Genetics, Electrophysiology, Center for Better Health and Nutrition, Fontan Management, Cardiomyopathy, Cardiac Rehabilitation, Pulmonary Hypertension, Neurodevelopmental and Education Center, Preventive Cardiology, General Pediatric Cardiology, Fetal Cardiology, Syncope, and Cardiothoracic Surgery Consultations.
A Business Development Manager within the HI was assigned as the point of contact to work with TCT, the Scheduling Center, and the clinical teams. Once assigned a TCT Consultant, the pre-visit planning, scheduling, and workflows were developed, and formalized trainings were scheduled to prepare the clinic teams for go-live. After the department requests were submitted to TCT, individual programs were ready to launch within 7 days of the telehealth request submission.
Scheduling Processes
Cardiology patients are often less appropriate for telehealth compared to other specialties due to the need for imaging and auscultation during physical exam. As such, cardiologists reviewed schedules and identified patients who were appropriate for a telehealth visit. A nurse or care coordinator would then call the patient to confirm they were comfortable being seen via telehealth. Upon approval, the nurse or care coordinator sent the date and time of the appointment, if it would be an audio or video visit and updated contact information to the scheduling center.
The process for identifying patients appropriate and willing to have telehealth visits was very manual and cumbersome. As a result, a disposition in Epic was created for the provider to flag whether a patient is appropriate for telehealth visits in the future.
Training and Onboarding
A telehealth workflow was developed for each clinical program to illustrate step-by-step roles and responsibilities from pre-visit planning and scheduling through documentation and billing for the visit. A designated TCT trainer conducted technical trainings to familiarize the providers with how to utilize the telehealth software platforms. To manage the volume of providers requiring onboarding, the trainer created 3 instructional videos and 13 job aides to augment the virtual training sessions. Implementation involved training over 70 different staff of varying disciplines in the HI [Figure 3].
Methods
Telehealth Platforms
Telehealth visits at CCHMC are conducted via video visit using Cisco Jabber or Microsoft Teams. Jabber is used for one provider to connect with a patient, parent, or guardian. Microsoft Teams is used for multi-party visits for either more than one provider or for when parents are in two locations. Schedulers indicate in the appointment notes which type of platform will be used for the visit. Initially, sending the links to patient families and providers was a very manual task.
TCT developed a scripted email for divisions to send to patients that included instructions on how to download the free app onto their device, test their connection and the link for their scheduled telehealth visit. Job aids were shared with divisions on the following topics:
- Changing a scheduled in-person clinic visit to a telehealth visit
- Downloading and using Jabber and Teams
- Documenting a telehealth visit
The process of emailing patient families was automated shortly after implementation. Links were automatically emailed two days prior to the visit to the preferred email listed in the Epic patient demographics. Schedulers were instructed to indicate either VIDEO or AUDIO in the appointment notes. Links were sent for the visits that were scheduled for VIDEO, as AUDIO would just be a telephone call at the appointment time.
To streamline processes, hospital leadership asked divisions to select a single telehealth platform to utilize. Due to several multidisciplinary clinics employing telehealth, the HI transitioned to using Microsoft Teams in June of 2020. To increase efficiency, accuracy and interoperability, sending Microsoft Teams links to patients has been automated and the scheduled visits appear on provider’s Epic calendars. Most importantly, to continually improve and address any issues, feedback from providers and clinicians was encouraged on processes, user training, and job aids.
Challenges
Volume-Induced Process Variability
CCHMC scaled telehealth visits in patient homes hospital-wide, creating capacity constraints due to a 100-fold increase in telehealth patient visits. Implementation required strong collaboration across divisional leadership, the Scheduling Center, TCT, MSS, and the individual programs launching telehealth. Due to capacity constraints and cross coverage, there were inconsistencies across programs for tasks such as creating the link, scheduling the telehealth visit in Epic, and contacting the patient. As processes were further refined and improved, there were challenges with effectively communicating the frequent updates and how to best manage this without triggering email fatigue amid all the other COVID updates coming out.
Provider Licensure Across State Lines
State licensure regulations have long been a barrier to telehealth expansion. CCHMC is in a tristate border area (OH, KY, IN), where differing laws and licensure requirements across the three states created confusion during COVID-19. For example, Indiana did not waive the Registered Dietician (RD) state license requirement, impacting care to CCHMC’s Indiana patients who live just across the border. As a result, multidisciplinary clinics involving a RD involved a separate phone call from the physician visit and an unbillable RD visit documented in Epic as a telephone encounter. Operationalizing telehealth required different approaches to care based on the patient’s state of residence and the type of provider.
Navigating a New Care Model
Additional challenges centered around the telehealth infrastructure and interoperability with Epic, and the patient dynamic when implementing a new care model. Most providers were utilizing Teams for the first time and unlike in-person visits, initiating the telehealth visit occurred outside of Epic for the first four months. Further, patients who were not familiar with telehealth often did not test their device or read instructions in advance of the visit, leading to last minute attempts to resolve connectivity issues. Common issues included:
- Patient not receiving the email with their appointment link for varying reasons:
- The email went to the patient or family members spam folder.
- Email address listed in Epic was not correct or their primary contact.
- The patient was scheduled less than 48 hours prior to their appointment and TCT team wasn’t notified.
- Patients incorrectly scheduled for a telehealth visit were not arrived for the visit, disrupting clinic flow.
- Computer or software issues – patient and provider not able to see and/or hear each other.
- Provider not logged on to system when the patient tried to connect, so patient received an error message.
- Provider logged into system via a web browser with limited capabilities versus the application with full system access.
- Canceled and rescheduled visits caused confusion because Epic and the telehealth platforms were not initially synched. The change must be reflected in both platforms to ensure everyone was notified.
Staffing Impacts
Due to the initial influx of telehealth utilization hospital-wide, trained resources were scarce. As such, some HI Administrative and Nursing staff stepped outside of their normal scope of work by learning the scheduling and telehealth functions, including sending patients and families telehealth instructions and the link to connect to their telehealth visit.
There were some areas within CCHMC where employees could not return to work and work was not able to be transitioned to home. This included auditing staff from the scheduling center and registration personnel. There were 5.0 full time equivalents (FTE) of staff who were temporarily redeployed to assist TCT in answering incoming patient and provider calls, as well as manually sending patient instructions until the process could be automated. This was in addition to 2.0 FTE from TCT who temporarily were moved to these daily operations duties. Three permanent positions have since been added to accommodate long-term volume change.
Tactics to remedy the challenges involved centralizing coordination of telehealth across the HI to a key contact, including submission of division request forms to TCT for each clinic and a formalized training with a TCT consultant. Prior to launch, the key contact worked with MSS on ensuring all licensing requirements were met. And post-implementation, the key contact worked with the Scheduling Center to run and audit a list of telehealth visits scheduled daily to ensure the visit type and appointment note were complete and accurate.
Results and Future State
Telehealth Volumes
In-home telehealth volumes for the HI increased from an average of 3 visits per month up to a maximum of 546 visits in May, an 18,100% increase [Figures 4 and 5]. Since COVID-19 and CCHMC’s response in March, telehealth visits accounted for 20.4% of all HI outpatient volumes. Between March and May 2020, in-person volumes were limited to 50% capacity to accommodate social distancing. In June 2020, in-person clinic capacity increased to 75% and back to 100% in July 2020 with a strong recommendation to aim for 1-2 telehealth visits per in-person clinic, when possible. Between March and June 2020, there was a 43% drop in in-person visits compared to pre-COVID-19 but with the utilization of telehealth, overall outpatient volumes only decreased by an estimated 28% of normal volumes.
Prior to the first reported case of COVID-19 in Ohio in March 2020, 42 specialties were providing care via telehealth. In a typical year, CCHMC’s telehealth volume is roughly 1,400 patient visits. Between July 2019 – February 2020, 1,730 visits occurred and 56% of those were in the patient home. Those numbers dramatically changed for the remainder of Fiscal Year 2020. The number of specialties providing telehealth visits rose to 78, and the total volume of completed visits by the end of June 2020 was 85,023. Ninety-nine percent of the visits were being completed in patient homes.
Patient and Family Experience
During the pandemic, the HI was able to measure Patient Family Experience (PFE) scores for our medical and surgical divisions using telehealth. 84.4% of those surveyed ranked their visit a 9 or 10 on 10-point scale for overall experience, and the cardiology specific score was 81.1% (n=90) [Figure 6]. This is slightly lower than the ambulatory average of 87.7% and the cardiology average of 88.8% seen within the past year for in-person visits. The lower PFE ratings included comments around connectivity issues and not receiving the email with instructions and the appointment link. Comments from a few families indicated a preference to in-person exams due to their child’s condition, and those visits have been moved back to in-person as clinics re-opened.
Higher PFE ratings included comments on the ease of use, increased comfort for their child, and a significant reduction in length of visit. A telehealth appointment can be 15-30 minutes versus a 1 to 2-hour in-person appointment, when the commute, check-in and wait time are considered. Many families commented that they hope telehealth visits will be available after the pandemic as well. As processes improve and providers and patients alike become more comfortable with telehealth, a rise in PFE scores is to be expected.
Changes in Care Model
Due to COVID, telehealth was implemented rapidly across Divisions where providers would not have otherwise used telehealth. As a result, both providers and patients had the ability to test telehealth for themselves, leading to more buy-in among providers and patients for telehealth utilization moving forward. In CCHMC’s telehealth PFE surveys [Figure 6], 61.8% (n=102) of patients reported telehealth saved them money and 73.5% (n=102) reported that it saved them time. Quality of care, access and clinic volumes are maintained, while the cost (i.e., resources assigned to the visit) are less than the cost of an in-person visit. As such, telehealth reduces healthcare spending. However, many outpatient visits will require either partial or full return to in-person as the nature of cardiology care requires physical exams and diagnostic imaging of the heart. Some services such as Center for Better Health and Nutrition (CBHN), a nutrition and exercise therapy program, have remained at over 50% telehealth post-COVID, as many of those encounters provide coaching and program adherence between clinic appointments. There are advantages to seeing the patient and family at home and the impact to their health. Specifically, providers can see their exercise space and equipment, as well as the available nutrition within the home. Due to these findings and the success CBHN has had to date, the Cardiac Rehabilitation program has since implemented telehealth.
Telehealth Policy Reform & Coverage Expansion to Drive Sustainability
Pre-COVID, several telehealth restrictions created a barrier to expanded utilization: restrictions for providing care across state lines, originating site limitations, constraints on audio only telehealth, CPT Code reimbursement limitations, and the established relationship (in-person) requirement (SOC Telemed, 2020). Temporary policy changes during the pandemic mitigated these challenges by lifting restrictions on the types of care patients can receive from their home, permitting telemedicine to be provided across state lines, removing in-person requirements, and reimbursing telehealth visits similar to in-person services (Assistant Secretary for Public Affairs (ASPA), 2020). Post-COVID-19 telehealth policy and coverage changes, including making provisions in the CONNECT for Health Act permanent, will have a major impact on the long-term sustainability and scale of telehealth utilization (Wicklund, 2020).
Conclusion
In response to COVID-19, the HI at CCHMC shifted from two physicians utilizing telehealth to full implementation across 39 Providers, 24 Clinical Staff, and 10 Administrative staff in just 4 weeks. Further, telehealth volumes in the HI increased from 0.13% of outpatient volumes to 20.4% during the pandemic. Overall telehealth volumes for CCHMC increased from 0.22% to 33% from March- June 2020.
Rapid and expedited expansion of telehealth over a 4-week span that would normally take several months came with staffing, training, and technology challenges. Although some visits will shift back to in-person based on clinical need, the general perception of telehealth is perceived positively, and more providers, staff and patients are now more likely to use telehealth in the future. Studies show increased use of telehealth may reduce costs for patients and families, expand access to health care, and improve health outcomes (Pacific, 2020). Despite the value of telehealth recognized in research and by patients, families, and providers alike, telehealth policy and payor coverage expansion post-COVID-19 will be major driving factors for the expansion of telehealth services.
References
- Assistant Secretary for Public Affairs (ASPA). (2020, July 15). Telehealth: Delivering Care Safely During COVID-19. Retrieved July 21, 2020, from https://www.hhs.gov/coronavirus/telehealth/index.html
- Bischoff, L. A., & Spicker, K. (2020, May 13). Coronavirus timeline: A look at the orders changing life in Ohio. Retrieved June 16, 2020, from https://www.daytondailynews.com/news/local/timeline-coronavirus-prompts-orders-changing-everyday-life-ohio/gpnVSADPxZxMltlDVyqKEP/
- Centers for Medicare & Medicaid Services. (2020, March 17). MEDICARE TELEMEDICINE HEALTH CARE PROVIDER FACT SHEET. Retrieved July 23, 2020, from https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- SOC Telemed. (2020, April 13). Telehealth Restrictions Temporarily Lifted. Retrieved July 21, 2020, from https://www.soctelemed.com/blog/telehealth-restrictions-temporarily-lifted/
- Pacific Northwest Evidence-base Practice Center. (2019, April). Telehealth for Acute and Chronic Care Consultations. Retrieved July 21, 2020, from https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/cer-216-telehealth-final-report.pdf
- WCPO. (2020, April 24). Timeline: Coronavirus in Ohio. Retrieved July 21, 2020, from https://www.wcpo.com/news/coronavirus/timeline-coronavirus-in-ohio
- Wicklund, E. (2020, June 15). Experts Weigh in on Post-COVID-19 Telehealth Rules and Policies. Retrieved July 21, 2020, from https://mhealthintelligence.com/news/experts-weigh-in-on-post-covid-19-telehealth-rules-and-policies
Figures
Figure 1. Division Readiness Decision Tree for Telehealth.
- Group A: Divisions with an Epic build in place for scheduling telehealth visits; Providers experienced in telehealth could scale quickly as they only needed to shift scheduled patients from in-person to telehealth appointments.
- Group B: Divisions with an Epic build in place for scheduling telehealth visits; Providers in the division without telehealth experience required training and onboarding. This group would be ready to scale next.
- Group C: Divisions without an Epic build in place or providers trained for telehealth would take longer. Typical Epic builds took months to complete pre-COVID. An abbreviated Epic build was used to fast-track the process for 25 divisions who had no experience with telehealth.
Figure 2. COVID-19 Timeline in Ohio and at Cincinnati Children’s
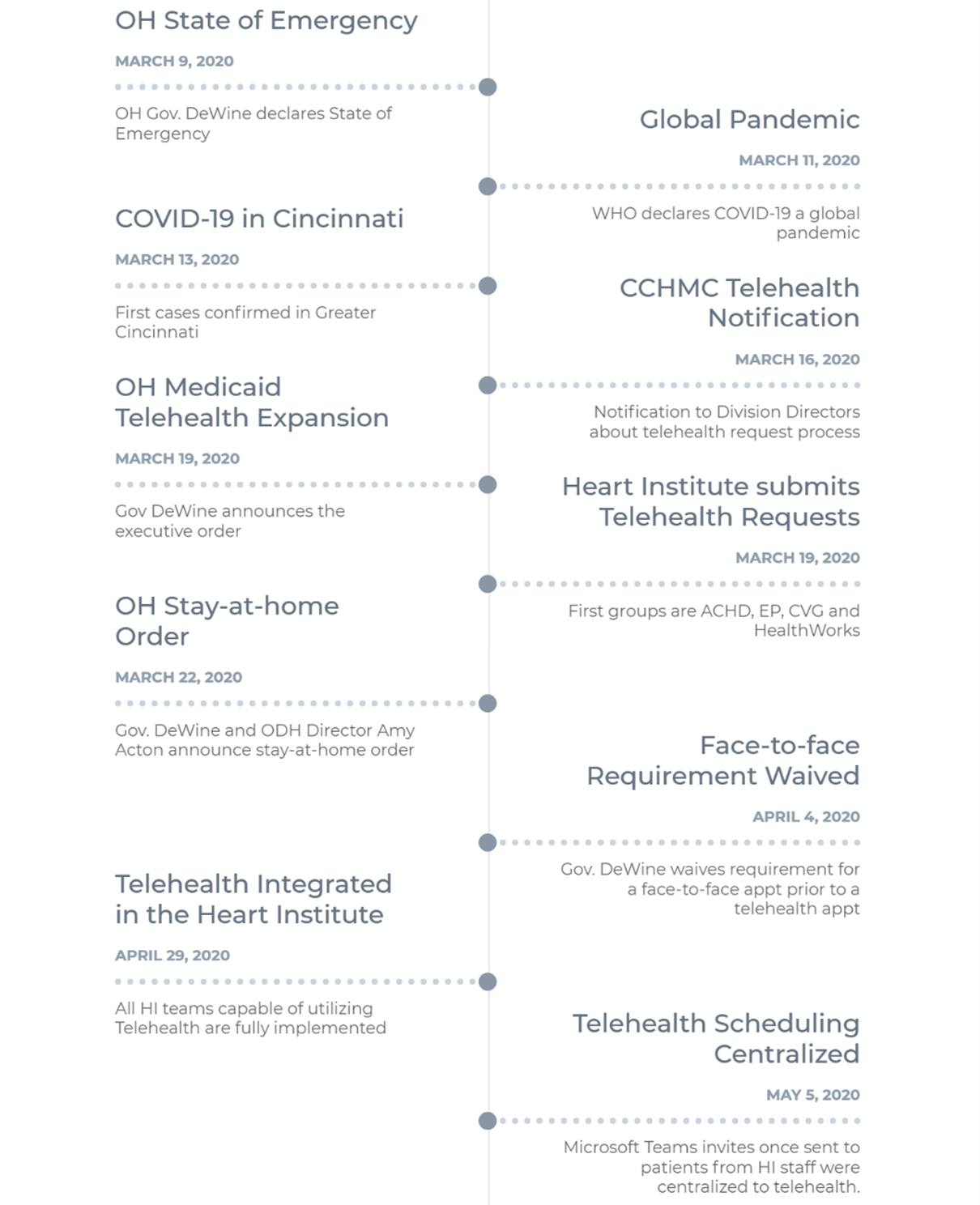
Figure 3. Cincinnati Children’s Heart Institute Staff Trained on Telehealth, March-June 2020.
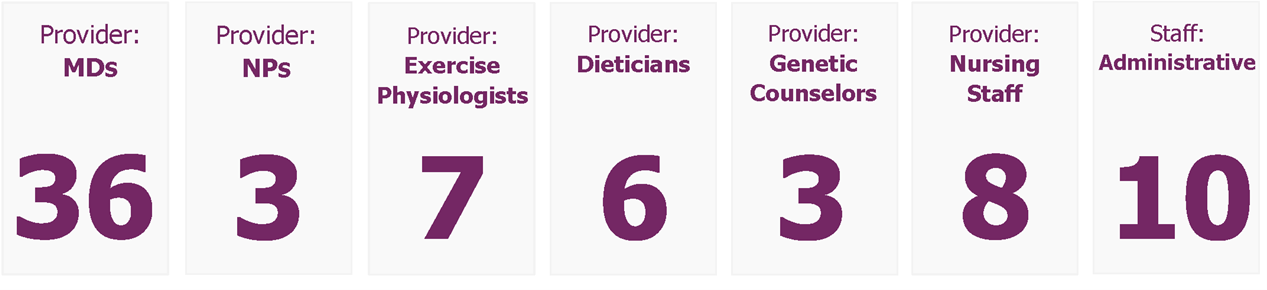
Figure 4. Total Telehealth Encounters in the Heart Institute, July 2019 – June 2020.
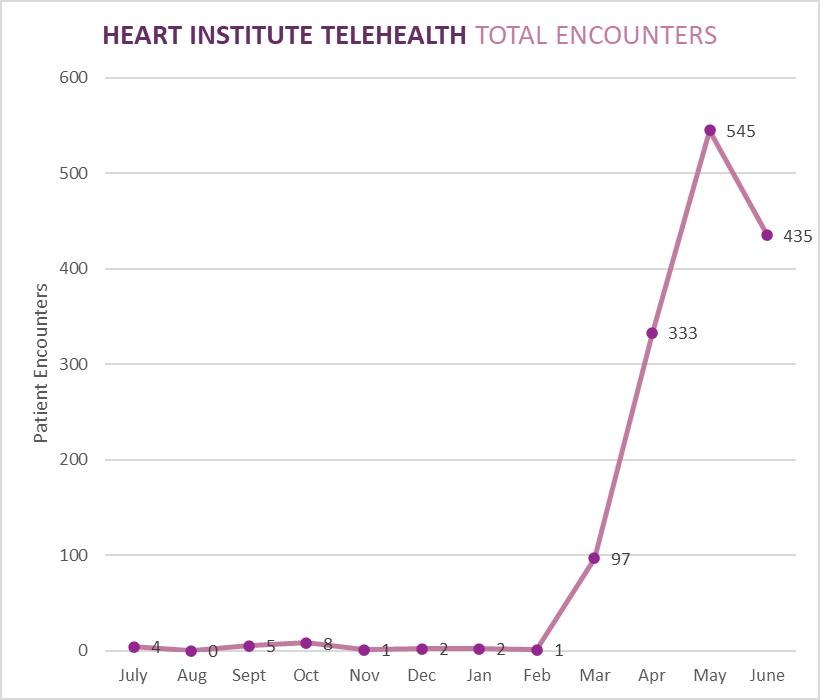
Figure 5. Total Telehealth and In-person Encounters in the Heart Institute, July 2019 – June 2020.
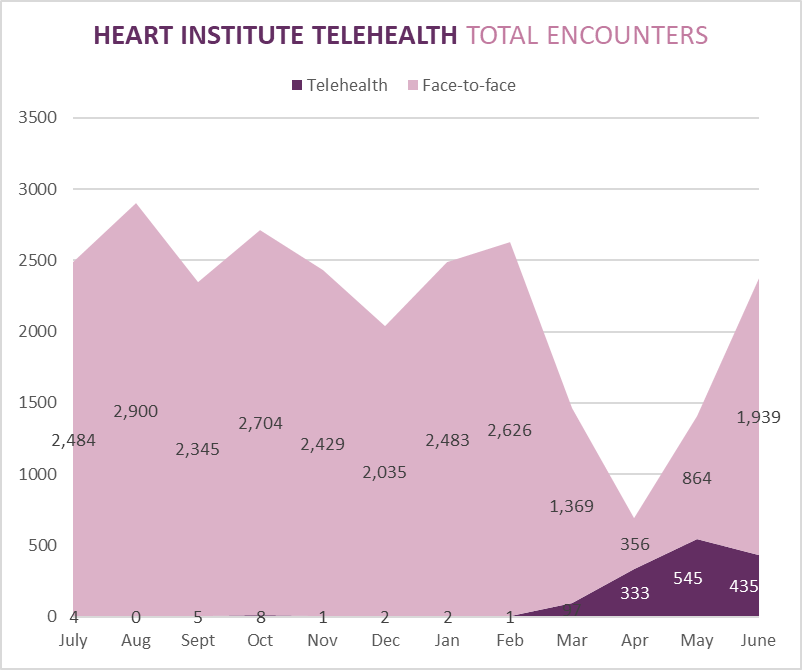
Figure 6. Heart Institute Patient and Family Experience Scores for Telehealth and In-Person Visits.