
Medicare Shared Savings Program Changes Bring Incentives to Form Accountable Care Organizations
By Deanna Kyrimis
Director, Health Care Consulting Practice
Moss Adams
Original Publish Date: May 7, 2019
The Affordable Care Act of 2010 (ACA) brought many changes to the health care system along with the sanction of a wide variety of delivery reforms. One of the most prominent delivery models now recognized by the federal government is the formation of Accountable Care Organizations (ACOs).
ACOs seek to provide a framework that allows providers to better coordinate care through incentives for quality over quantity. Even with these incentives, most organizations were hesitant to enter into these arrangements, and those that did struggled with the burden of maintaining the model. In 2012, 32 Pioneer Model ACOs formed, but only a handful remained just four years later.
Today, there’s been a resurgence in the number of ACOs with nearly 500 Medicare ACOs around the United States currently managing more than 10 million fee-for-service beneficiaries with an aim to:
- Better care for individuals
- Better health for populations
- Lowering growth in expenditures
Several factors can be attributed to this resurgence. The process of developing an ACO has become easier due to a more streamlined approach for filing paperwork with Center for Medicare & Medicaid (CMS), as well as a progressive loosening of application requirements that served as barriers. On December 21, 2018, CMS issued a final ruling for the Medicare Shared Savings Program (CMS MSSP). The ruling redesigned participation options and eased application filing requirements that previously prevented some health care organizations from participating in the program.
Under this model, health care organizations can collaborate, integrate, and ultimately transform from fee-for-service to a value-based care organization across the patient continuum of care. CMS ACOs are required to be led by physicians, with benefits for the physicians that include developing a clinically integrated network in partnership with hospitals and other entities designed to drive down cost while improving care and clinical outcomes.
Considerations for Forming an MSSP
With the barriers lifted, more organizations are contemplating the CMS MSSP model for several reasons. These include the desire to manage patients at the population level to target appropriate cost, high quality, and improved clinical outcomes, as well as to have a streamlined alternative to the regulatory reporting requirements by Medicare Access and CHIP Reauthorization Act (MACRA).
Benefits
The CMS MSSP model has several benefits including:
- Providing a glide path for evolving from fee-for-service (FFS) revenues to value-based risk models with shared savings distributions based on certain benchmarks
- Offering clinical integration for participants and other entities
- Developing care and cost transformation from the CMS MSSP chassis and extending them to other value-based arrangements to provide network scale and efficiencies
- Opportunity to pursue innovative mechanisms to control costs
- Engaging physicians in a clinically integrated gain-sharing model that transforms their physician payment system to one that promotes quality performance and engagement
Goals
MSSPs are designed to bring together voluntary participants such as physicians, hospitals and long-term care facilities for the purposes of coordinating care and allowing patients, especially the chronically ill, to get the right care at the right time while avoiding unnecessary duplication of services and preventing medical errors.
The collective goal of an MSSP is to work together to improve care delivery and clinical outcomes through:
- Promotion of accountability for quality, cost, and overall care of a Medicare patient population
- Improved management and coordination of care for Medicare fee-for-service beneficiaries
- Investment in infrastructure and redesigned care processes for high quality and efficient service delivery
Eligibility
Those that can participate in CMS MSSP include:
- ACO professionals in group practice arrangements
- Networks of individual practices of ACO professionals
- Partnerships or joint venture arrangements between hospitals and ACO professionals
- Hospitals employing ACO professionals
- Critical access hospitals (CAHs) that bill under Method II
- Federally qualified health centers (FQHCs)
- Rural health clinics (RHCs)
- Teaching hospitals that elect to receive payment on a reasonable cost basis for the direct medical and surgical services of their physicians
A minimum of 5,000 attributed Medicare fee-for-service beneficiaries are a requirement for participation.
One- and Two-sided Risk Models
ACOs facilitate coordination and cooperation among health care providers to improve the quality of care for Medicare FFS beneficiaries and reduce the rate of growth in expenditures under Medicare Parts A and B. Under the MSSP reimbursement model, CMS will share a percentage of generated savings with ACOs that meet certain quality and cost performance standards. A CMS MSSP is held responsible for the total cost of care and quality outcomes for the assigned beneficiary patient population they serve.
Specifically, according to the CMS’ final rule, ACOs will receive a share of any savings they generate if they meet certain quality performance and program participation requirements. ACOs participating in a two-sided model must also pay CMS back if spending exceeds the benchmark. This means for ACOs participating in a one-sided model with no financial risk, the MSSP has the opportunity to share in savings generated if quality performance and program requirements are met. In a two-sided model where the organization takes on financial risk, there’s a possibility of owing money to CMS if spending exceeds certain benchmarks.
Organizations that haven’t historically excelled in managed care and a partial- or full-risk model may want to consider a one-sided model for laying the population health groundwork to then progress into a risk model and successfully manage the world of value-based contracting.
With the changes made to the CMS MSSP introduced late in December 2018, there’s a path to move from an upside only model with no financial risk to a downside model, with financial risk, over a period of two years; two and a half years if accepted for the stub period beginning July, 1, 2019. During this time, an organization can voluntarily terminate participation if needed.
Collaboration Using CMS Waivers
Moving from volume to value is imperative in today’s world of health care, but this can’t be done without breaking down barriers to collaboration. A significant benefit of participating in an MSSP is the opportunity to use the CMS fraud and abuse waivers to overcome barriers and develop deep clinical integration in the care continuum.
Under the MSSP, CMS will waive certain fraud and abuse laws—CMS MSSP must follow specific requirements to enact the waiver—that can result in a more favorable legal environment to develop relationships, programs, and reimbursement mechanisms.
Waivers allow for collaboration that can create aligned incentives to:
- Control costs
- Develop redesigned care processes
- Implement across-the-system efficiencies
- Manage and coordinate care to improve population management
- Maintain and improve quality while accomplishing all of the above
Waiver Types
There are two key waivers, pre-participation and participation waivers.
A pre-participation waiver overrides Stark and Federal Anti-kickback Statute (AKS) with respect to start-up arrangements that predate an ACO's participation agreement with CMS.
A participation waiver overrides Stark and AKS with respect to any arrangement of an ACO, one or more of its ACO participants, or its ACO providers and suppliers, or a combination of both.
Participation and use of the CMS waivers allows for thoughtful and true physician alignment that promotes accountability for quality, cost, and overall care of patients. Additionally, there’s a mechanism to legally reward providers for Triple Aim value that’s above and beyond a Medicare Shared Savings reimbursement or traditional medical directorships, management service agreements, or salary and productivity payment models.
While the waiver opportunities are significant, another benefit worth highlighting is that as an MSSP participant, organizations will find relief from MACRA reporting burden requirements and submission as the MSSP is required to submit the quality data as part of its participation and on behalf of the participants.
When contemplating the future and moving into a value-based model, CMS MSSP provides an innovative model for managing the health and well-being of a population at an appropriate cost while improving clinical outcomes. Pair that opportunity with the CMS waivers, and the work of transformation isn’t only attainable, but also tangible.
CMS MSSP Case Study
In 2016, a multi-specialty physician group in Southern California set out to start its own CMS MSSP. The group comprised of approximately 75 physicians and affiliated with three major hospitals in their service area with 10,000 attributed Medicare beneficiaries. This physician-led ACO saved $6 million and earned a shared savings distribution of $3 million in their first year. An annual overview of their activity follows.
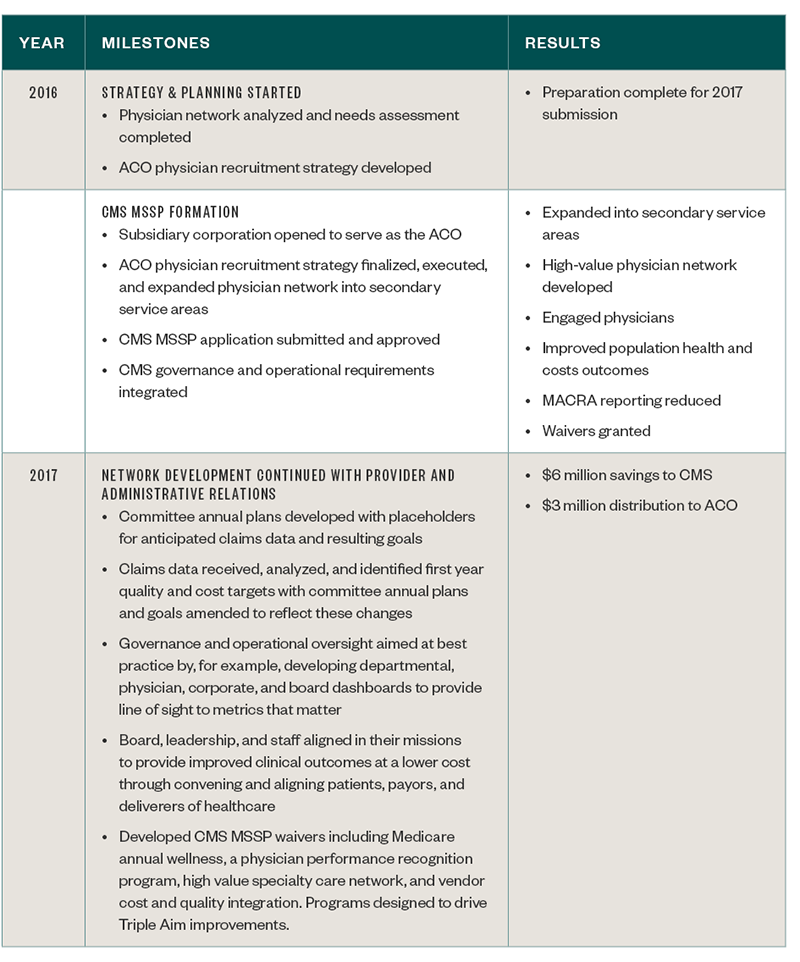
Benefits
By starting its own CMS MSSP, the physician group experienced several positive outcomes including expanding into secondary service areas and creating a high-value physician network that served an expanded patient population in its mission to provide high quality care with improved outcomes at an appropriate cost.
They greatly reduced the MACRA reporting and administrative burden to physician participants. Patient engagement enhanced through a newly-formed patient advisory committee, and physician satisfaction also improved as waiver programs were rolled out to support their journey in value-based care and help underwrite associated cost to meet the three-part aim. The ACO convened physician and hospital networks to collaborate, innovate, and transform care delivery through the appropriate use of the CMS MSSP waivers.
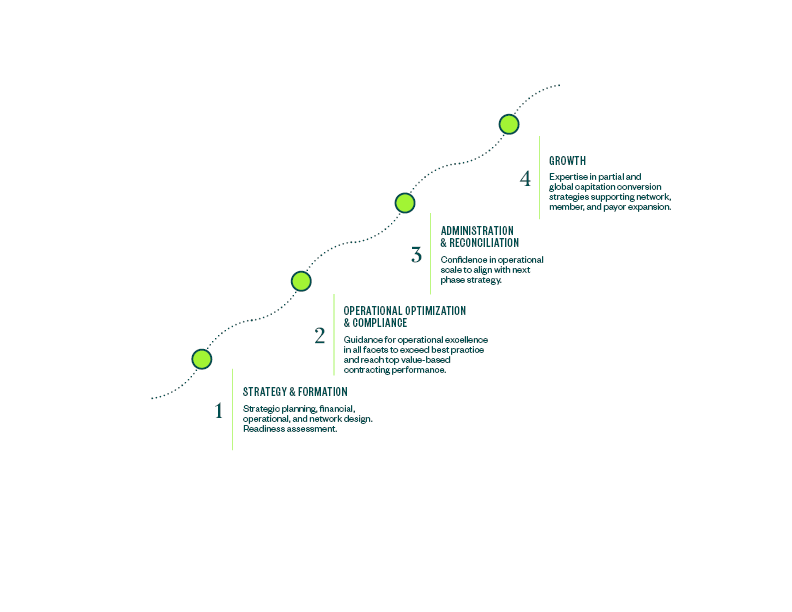
Next Steps
A CMS MSSP can develop a provider network that’s designed to collaborate, innovate, and transform health care that moves beyond the boundaries of a traditional network. CMS waivers are able to break down traditional barriers while providing a clinically integrated mechanism to expand high value networks and deliver the highest quality of care to the patients being served. Navigating your organization throughout the shift from fee-for-service to risk, as shown below, can be a complex process. Working with a third-party advisor with expertise in the field can help guide you through the transformation in a smooth manner.
Managed Care Cycle
Deanna Kyrimis is a director for Moss Adams Health Care Consulting Practice with more than 20 years of experience in the health care industry focusing on specialty and multi-specialty physician organizations. Her expertise includes hospital and physician growth market strategies and clinical integration and business innovation models, specifically ACOs driving the Three Part Aim and MSOs, that help diversify revenue sources and provide efficiencies and scale. She can be reached at (858) 627-5532 or deanna.kyrimis@mossadams.com.