
Creating a Quieter Hospital: Enloe Medical Center 2009-2014
By Marcia Nelson, MD, MMM, CPE, FAAFP, FACPE
Vice President of Medical Affairs
Enloe Medical Center
Read PDF of this article See all this Month's Articles
Original Publish Date: July 07, 2014
Enloe Medical Center has been on a long journey towards creating a quieter environment for our patients. In 2009, close to 35% of Enloe’s patients said their hospital room was “always” quiet at night. That put Enloe in the lowest 5% in the country. Granted, the majority of patient care occurred in a tower built in 1980, with hard surfaces and increasingly crowded nursing stations. Patients usually shared a room with another ill person. In that environment, however, awareness about the restorative effect of quiet on patients and staff was lacking.
In 2006, Enloe became a Planetree affiliate, aspiring to create a more patient-centered experience throughout the organization. Efforts began to improve performance on the recently released HCAHPS measures. Our new Planetree Leadership Team created the Quiet Hospital Task Force which embarked on a journey to make an impact on the noise level in the hospital. Enloe was also planning the new Magnolia Tower, slated to open in 2012, with design elements and materials intended to create a calmer, quieter space.
Early Work
Early work involved educating staff about the impact of noise on healing in order to demonstrate the need for change. Recorded and printed Senior Team messages raised awareness that patients healed faster and had better immune function when hospital noise is not excessive. Staff burnout is also less in quieter environments. We reported that a one-day decibel monitoring study revealed a minimum noise level of 65 decibels (as loud as a busy street) and at worst, it registered 108 decibels (as loud as a subway station).
We looked at some “low hanging fruit” for early successes and refashioned the loud air curtains on outside doors. We removed loud music in the Emergency Department. Engineers started to hear about squeaking wheels and other noisy equipment. Medical staff pages were routed by the operators to cell phones or pagers rather than announcing them overhead, and staff commented that the lower noise level made it feel more like a calm weekend. A barrier to overcome was some physicians’ reluctance to share their cell phone numbers, concerned that the information might be divulged to callers. A commitment to safeguard the phone numbers was instrumental to the success of this project.
We also employed visual cues to give some feedback on noise levels. “Yacker Trackers”, stoplight-appearing devices that respond to noise levels with red/amber/green lights, were placed in nursing stations. These only had a finite benefit and, once staff realized they could change the settings so the red light would not be triggered, we realized this was not a long term strategy.
The 2012 Quality Initiative
In 2012, we reenergized our efforts to create a quiet environment for our patients. Since 2009, Enloe’s quality calendar revolves around an annual Quality Summit at which three to five quality initiatives are selected for the upcoming year (see “Creating a Quality Movement in Your Hospital” California Healthcare News Sept 2010). At the April 2012 Quality Summit, Protecting Patients’ Sleep was named one of the year’s quality initiatives.
The year-long project included patient focus groups, creating “Sleep and Rest Guidelines”, stopping floor buffing at 2030 and dimming the unit lights every day between 1400 and 1500. Nurses bundled care to minimize the number of interruptions at night. Communication guidelines included recommendations about cell phone use and hallway conversations. A “Hush Line” was created so that patients could report loud noises. A popular addition has been the Sleep Menu from which patients can select items such as aromatherapy and sleep masks. Engineering was able to change the process for the weekly 0400 generator check so that hospital doors no longer slam shut.
Staff was also invited to participate in the Protecting Patients’ Sleep Challenge. A Yacker Tracker “patient” was placed in a bed to register noise above 50 decibels and staff had to perform routine care such as emptying a commode hat and drawing the bed curtains. Interestingly, the “snap” of putting on gloves was one of the noisiest tasks. This challenge is an engaging way to raise awareness of the noise created during the provision of care.
The Magnolia Tower
Since November 2012, patient care has occurred largely in the new Magnolia Tower. With sound absorbing surfaces, more spacious and less congested nursing stations and private patient rooms, the new tower is about 1/3 quieter than the 1980 tower. Some suggestions from our patients led to creating dark screensavers for the bedside medication workstations so that the light does not disturb sleep. Also, quieter paper towel dispensers were installed. The 1980 tower is being remodeled to include the sound-minimizing materials included in the Magnolia Tower and work stations are redesigned to reduce staff congestion.
Where is Enloe Now?
After many years of focused effort, Enloe’s patients report that their rooms are “always” quiet at night over 60% of the time. This puts Enloe above the national average and, while not yet at our goal of top quartile achievement, it is significantly better than our 2009 performance.
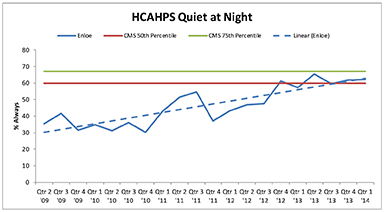
Of note is that, while moving into the Magnolia Tower has significantly contributed to this progress, the Quiet at Night scores were improving before that transition. Increased staff awareness and a renewed focus on delivering patient-centered care were the catalysts for the gains made since 2012. Our next steps include holding another round of the Protecting Patients’ Sleep Challenge. The new Patient-Family Advisory Council will be asked for input on further improvements, and staff education will be updated. Success on this metric is steady but slow. With the involvement of physicians, staff, patients and families, cultural transformation will continue, resulting in a quieter, patient-centered environment.
Marcia F. Nelson, MD, MMM, CPE, FAAFP, FACPE is a practicing family physician in Chico, California. Since 2005, she has been the Vice President of Medical Affairs at Enloe Medical Center. Dr. Nelson has been instrumental in leading her hospital from crisis to being recently named by a national publication as one of the top ten hospitals in the country for safe surgery. Central to that success is developing strong physician leadership which is showcased in the annual Quality Summit, created by Dr. Nelson in 2009. The California Hospital Association awarded Dr. Nelson the Ritz E. Heerman Memorial Award (2012) in recognition of her contribution to patient care in California. Dr. Nelson has delivered presentations on physician-led quality improvement to the Planetree Annual Conference and the California Hospital Association. Her work on this topic was published by the American Journal of Medical Quality (2013).
Dr. Nelson graduated magna cum laude from California State University, Chico and earned her medical degree from UCLA. After receiving her MMM (Beta Gamma Sigma) from the University of Southern California in 2012, she earned her CPE in 2013. Dr. Nelson is board certified in Family Medicine and is a Fellow of the American Academy of Family Physicians and the American College of Physician Executives.