

Understanding the Nuances of the No Surprises Act Good Faith Estimates
By Lori Laubach
Partner, Health Care Consulting Practice, Moss Adams
By Mandy Mori
Senior Manager, Health Care Consulting Practice, Moss Adams
Original Publish Date: September 6, 2022
Passed in 2020 and effective January 1, 2022, the No Surprises Act contains provisions that protect people from surprise medical billing and out-of-network emergency care costs not reimbursed by insurance. The law requires that providers and facilities send eligible uninsured or self-pay patients a good faith estimate (GFE). The GFE should detail as best as possible the charges patients can expect for scheduled visits, tests, supplies, drugs, or other services based on the expected course of treatment.
- No Surprises Act GFE requirements, eligibility, and timing
- Information to include in the GFE
- Posting the good faith estimate notice
- Mitigating risks with workflow adjustments
- Scenarios to watch for
- Does your good faith estimate have what it needs?
No Surprises Act Good Faith Estimate Requirements, Eligibility, and Timing
with other elements of the No Surprises Act, the scope of the GFE requirement is expansive. Many providers may be subject to it without realizing it.
Who’s Required to Provide Good Faith Estimates?
GFE rules apply to health care providers and facilities, including physicians, air ambulance services, hospitals, outpatient clinics, labs, imaging centers, and much more. The GFE can also apply to ancillary providers, such as dentists, chiropractors, cosmetic plastic surgeons, acupuncturists, behavioral health specialists, and physical, occupational, and speech therapists.
Who Is and Isn’t Eligible for Good Faith Estimates?
Uninsured patients should be informed regarding their eligibility to receive GFEs orally or in writing, as well as individuals who otherwise have insurance but choose instead to self-pay.
Health care providers aren’t required to provide a GFE to those covered by Medicare, Medicaid, Indian Health Services, Veterans Affairs Health Care, and Tricare.
When Is a Good Faith Estimate Required?
Providers should send GFEs when a patient has a primary item or service that’s scheduled for a date outside the current period of care - admission through discharge for hospitalizations, and day of care for outpatient visits.
Qualifying items and services can include:
- Encounters
- Procedures
- Medical tests
- Supplies
- Prescription drugs
- Durable medical equipment
- Facility fees
Self-pay or uninsured patients may also request a GFE when shopping for an item or service, such as when they want to compare imaging prices from one center to another.
How Soon Should the Good Faith Estimate Be Sent?
The No Surprises Act stipulates that GFEs are sent according to a strict schedule:
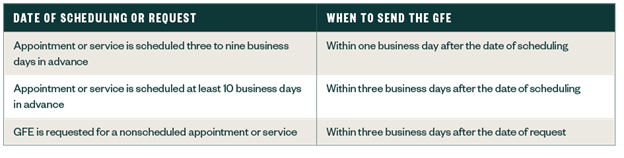
- If the appointment or service is scheduled three to nine business days in advance, send the GFE within one business day after the date of scheduling.
- If the appointment or service is scheduled at least 10 business days in advance, send the GFE within three business days after the date of scheduling.
- If a GFE is requested for a nonscheduled appointment or service, send the GFE within three business days after the date of request.
Date of Scheduling or Request versus Date of Appointment
Remember that the date of scheduling is the day that the future item or service gets booked into the appointment calendar, and the date of request is the date that patients ask a question - any question - related to payment. GFE timelines apply to either the date of scheduling or the date of request, not the scheduled date of service.
The clock starts at the point of scheduling, and deadlines work forward from there. This may mean that GFEs get sent weeks or months before a surgery, for example. If a patient is uninsured or chooses to self-pay at the time of scheduling or request for GFE but is later expected to become insured, a GFE is still required.
Information to Include in the Good Faith Estimate
GFEs contain itemized details about the primary item or service as well as the expected charges for anticipated services in the care plan or the individual’s expected course of treatment. GFEs must be delivered in written form, either on paper or electronically, and must follow a verbal notice.
Be specific. While GFEs aren’t perfect, the name “good faith” implies just that. They are an honest effort and should meaningfully account for foreseeable changes, not just generically estimate or bundle prices.
What Should a Good Faith Estimate Include?
The Department of Health and Human Services (HHS) has provided a GFE template that can be helpful, but isn’t required. If you choose to create your own GFE, be sure to include the following:
- Patient’s name and date of birth
- Clear and easy-to-understand description of the primary item or service with the scheduled date of the primary item or service, if applicable
- Itemized list of items or services as part of the treatment, grouped by each convening and co-provider or facility, to be provided during a defined period of care
- Diagnosis, expected service codes, and expected charges associated with each listed item or service provided during a defined period of care
- Name, National Provider Identifier (NPI), and Tax Identification Number (TIN) of providers involved in the treatment
- Specific disclaimers noted in the HHS example
A provider can issue a GFE for recurring primary items or services if the GFE clearly and understandably describes the expected scope of the recurring primary items or services (timeframes, frequency, and total number) and doesn’t exceed 12 months.
What Are Expected Charges?
The expected charge is the amount providers would charge cash payers, or the rate otherwise reserved for uninsured or self-pay patients - inclusive of discounts or adjustments.
Posting the Good Faith Estimate Notice
Much like the Health Insurance Portability and Accountability Act (HIPAA) Notice of Privacy Practices, all providers should post the required No Surprises Act GFE notice for uninsured and self-pay patients on their websites and in-person locations. HHS has developed a model notice in its downloadable resource package for providers’ use.
At the same time, providers should post the separate required notice about surprise billing for out-of-network services. HHS has also developed a model notice for this one. The first installment of our NO SURPRISES ACT Implementation Guide further addresses those requirements.
Mitigating Risks with Workflow Adjustments
As with any law of this scope, organizations should consider workflow adjustments as they prepare for GFE requirements. Adjustments can help mitigate certain risks, like sending the GFE too late.
Timing
The American Hospital Association (AHA) estimates that it takes 10 to 15 minutes to make a single GFE. Estimates should go out no later than three days after scheduling, depending on the date of appointment. With this fast turnaround, the AHA has noted that facilities need to make operational and workflow changes to comply with the requirement—not just to send GFEs out, but also to monitor compliance systemwide.
How to Mitigate
Process, process, process. Providers should establish a clear and repeatable procedure detailing how GFEs will get completed and sent on time, preferably codifying it into formal policy. They should also designate a team with oversight to generate GFEs, send them out, and receive requests.
One potential problem is a lack of controls over which personnel can make appointments when they don’t have the responsibility to generate GFEs. This means communication between the scheduler and the team authorized to generate GFEs is key.
As the AHA notes, automated systems may help expedite some tasks. However, because GFEs are quite customized, complete automation may not be possible.
Internal Controls
Given the manual or semi-manual nature of GFE generation, variations will be inevitable if internal controls aren’t in place to standardize GFE workflows.
How to Mitigate
Establish internal controls and policies around generating the GFE and monitoring compliance. Use reporting and alerting tools at the point of scheduling to alert the scheduler or other staff that a GFE is required, as well as a form to generate the GFE. Developing tools that assist in preparing for routine services can facilitate workflows while mitigating variation.
Staff Training
As workflows adjust, training gaps can further drive variation and noncompliance risk.
How to Mitigate
Ensure that trainings and tools get equally distributed across the workforce and cover various areas, from generating the GFE to communicating about it to patients. In addition, make training more dynamic: It should adapt with workflow modifications and regulation changes.
Estimate Ranges and Complexity
While specificity is the gold standard, a range of costs may sometimes be acceptable for the GFE. As the Centers for Medicare and Medicaid Services (CMS) have indicated, an organization should try to capture all charges.
Some providers, like psychiatrists, may not know how much care planning new patients will need. If you provide a range, try not to make it too big of a range which could pose a compliance risk.
How to Mitigate
Create a policy detailing how to approach ranges, such as identifying factors that could result in the lower or higher ends of the range. For example, a psychiatrist might recommend between 10 and 25 sessions at 50 minutes each within a given year, listing a charge at a given rate per session and what that is expected to total at the end of the year.
In highly complex cases communicate with the patient. Understanding their preferences for an item or service - such as whether they want stainless steel or porcelain crowns for dental work, for example - may help narrow the scope of any applicable ranges.
Co-provider and Co-facility Collaborations (for 2023)
A single GFE should account for the mix of in-house providers, consultations, and follow-up care required for a given course of treatment. After all, the intent is to give patients the full picture of costs for a particular health care event.
However, comprehensive care often involves other providers and facilities. This may mean that the facility or provider who schedules the item or service—known as the convening provider—will have to collaborate with co-providers and co-facilities to determine what should go into the GFE. While this specific rule doesn’t take effect until January 1, 2023, it’s a good idea to plan for it now.
How to Mitigate
Collaborate with co-providers and co-facilities now to prepare for how the group will comply with the Phase 2 regulations in January 2023. Have discussions to get familiar with the components that contribute to an accurate GFE. Consider implementing and testing before the due date. Establishing rules of the road prior to the due date to ensure turnaround times, staff training, and controls may be helpful.
Scenarios to Watch for
As with other aspects of the No Surprises Act, the rules around GFEs are nuanced. The below scenarios emphasize just how far the law’s scope extends.
What If There Is No Expected Charge?
GFEs will still be required. There are no minimum qualifying payment amounts. Expected charges of the GFE include estimates of no financial responsibility—such as when the provider anticipates a $0 price.
What If You’re a Dentist, Physical Therapist, Chiropractor, etc.?
The No Surprises Act affects providers licensed to provide scheduled health care services. If you schedule an item or service for a self-paying or uninsured patient—or if you’re asked to provide an estimate from a self-pay or uninsured person shopping for services—you’re required to send a GFE.
What If a Patient Loses Insurance Coverage After Scheduling the Service?
At the time of scheduling, always ask whether the individual is uninsured. If they are insured during scheduling but then lose coverage within three business days before the appointment, there is no requirement in the No Surprises Ac to provide a GFE or reschedule the appointment. But CMS does suggest that providers or facilities ask patients to report when their insurance information changes so that a new GFE can be issued if they become eligible before the appointment.
What If You Don’t Know Whether the Patient Is Self-Pay or Uninsured?
Providers are responsible for knowing the patient’s insurance status. Consider implementing changes to intake forms or scheduling scripts to confirm if patients are insured. If covered, ask directly whether they intend to self-pay for services.
What If the Good Faith Estimate’s Scope or Provider Changes?
If the provider or care plan changes, providers must send a new GFE within one business day before the scheduled item or service is rendered. The new provider must uphold the original GFE if the provider changes less than one business day before the scheduled item or service.
Does Your Good Faith Estimate Have What It Needs?
Organizations should assess GFE workflow changes, processes, policies, and internal controls when designing an internal audit to ensure they comply with No Surprises Act GFE guidance.
Refer to this list of things to look for:
- Has a policy and procedure been developed and implemented?
- What workflow changes have been made in scheduling and patient contact areas, such as the front desk?
- Is there a process for developing and provisioning GFEs?
- Is there a process to ensure data quality among GFEs?
- How will the GFE be tracked and monitored to flag needed updates or patient communications?
- What’s the plan to keep trainings updated and ongoing?
- Are internal controls and monitoring in place to ensure compliance with the No Surprises Act?
For More Information
GFEs - and the No Surprises Act at large - are fraught with complexity and risk for even the most well-prepared organizations. Contact your Moss Adams professional for help navigating these challenges and implementing workflows with compliance in mind.
You can also learn more about our Health Care Practice and additional topics affecting the industry.
Lori has been in health care consulting and public accounting since 1991. She has experience consulting for the private sector and not-for-profit organizations, including regulatory compliance program development and monitoring for integrated hospitals, multi-specialty clinics, single specialty clinics, mental health centers, and community health centers; forensic reviews; operational and revenue bench-marking projects; revenue cycle assessments; operational reviews; and risk assessments of physician groups and integrated systems.
Mandy has worked in the health care industry since 2003. She primarily works with health care executive leaders to drive strategic planning, service line optimization, and create sustainable financial growth. Mandy specializes in assisting clients with strategic analysis and development of internally integrated and externally oriented strategic plans that assess market demand, identify service gaps, and build clarity on the long-range strategic direction.
Assurance, tax, and consulting offered through Moss Adams LLP. ISO/IEC 27001 services offered by Cadence Assurance LLC, a Moss Adams company. Wealth management offered through Moss Adams Wealth Advisors LLC.